Our guide will help you gain a better understanding of medication adherence, why it's so important, and what you can do to address this significant challenge. Read the guide below or enter your email to download your copy to take on the go.
"Drugs don't work in patients who don't take them." This quote from C. Everett Koop, MD, former U.S. surgeon general, encapsulates the importance of medication adherence. When patients fail to adhere to their medication regimen by not taking their medications as prescribed, their health, wellbeing, and possibly even lives are put at risk. Poor medication adherence can also jeopardize outcomes and greatly affect overall healthcare costs. Unfortunately, statistics show that many people struggle with medication adherence. The reasons why are myriad and often complex. With adherence rates of 80% or more typically needed for optimal therapeutic efficacy, patients who are mostly adherent to their medication regimen can still experience significant health dangers.
While improving medication adherence is likely to be an uphill battle, it is one that providers and their organizations must embrace. And there are good reasons to do so. As the World Health Organization notes, "… increasing the effectiveness of adherence interventions may have a far greater impact on the health of the population than any improvement in specific medical treatments." Even small improvements can positively impact many patients' lives while reducing expenses and improving provider and staff productivity. As the scale and scope of improvements grow, so will the number of affected patients, and thus the gains achieved by providers and their organizations. Consider this e-book a roadmap you can use to gain a better understanding of medication adherence, why it's so important and so difficult, and what you can do to make headway on addressing this significant challenge.
Medication adherence is often identified by its shortcomings, which include suboptimal outcomes, higher rates of hospital admissions, increased morbidity and mortality, and rising healthcare costs. In fact, out of 4 billion prescriptions written annually, one in five new prescriptions are never filled.
Before we explore the many issues related to medication adherence, let’s discuss what it is, a few ways it’s traditionally defined, and some of the most significant challenges healthcare providers face when working to achieve medication adherence.
While many organizations define medication adherence slightly differently, each of the below definitions expresses a similar meaning.
"Medication adherence, or taking medications correctly, is generally defined as the extent to which patients take medication as prescribed by their doctors. This involves factors such as getting prescriptions filled, remembering to take medication on time, and understanding the directions."
"A patient is considered adherent if they take 80% of their prescribed medicine(s). If patients take less than 80% of their prescribed medication(s), they are considered nonadherent." (Source)
"Medication adherence occurs when a patient takes their medications according to the prescribed dosage, time, frequency, and direction."
Now that we’ve reviewed the definition for medication adherence, let’s explore some of its top challenges.
It’s vital for providers to understand each of these issues related to medication adherence so you can easily recognize them and find solutions for patients dealing with such challenges. Later, we’ll share the many opportunities to improve medication adherence, which include ways to prevent medication nonadherence.
We’ve already been discussing the term medication adherence in this guide, but what does it mean when someone refers to medication compliance? While subtle, let’s take a look at medication adherence vs. compliance.
There are four major ways these two terms can differ, including definitions, risks, causes, and improvements.
As defined by the National Stroke Association:
A Podiatry Today article further differentiates between the concepts, stating, "Adherence is an active choice of patients to follow through with the prescribed treatment while taking responsibility for their own well-being. Compliance is a passive behavior in which a patient is following a list of instructions from the doctor. Adherence is a more positive, proactive behavior, which results in a lifestyle change by the patient, who must follow a daily regimen such as wearing a prescribed brace. In contrast, compliance is a behavior exhibited by a patient who is simply "doing as (he or she is) told" or following a list of instructions given by the treating doctor."
While there is some overlap between the risks involved with medication adherence and compliance, there are also a few distinctions.
When it comes to medication adherence, 20-30% of prescriptions are never filled, according to an Annals of Internal Medicine review. Ultimately, poor medication adherence can lead to risks such as:
As for medication compliance, a survey sponsored by the National Community Pharmacists Association and conducted among American adults 40 and older who have been prescribed ongoing medication for a chronic condition found that about 28% of patients failed to refill a prescription in time, 57% of patients missed a dose, 22% took a lower dose, and 14% stopped taking their medication. These issues can lead to risks such as:
The causes of medication nonadherence and noncompliance vary widely. Causes of medication nonadherence include patients not filling prescriptions due to cost, access to a pharmacy, and challenges with tracking refills.
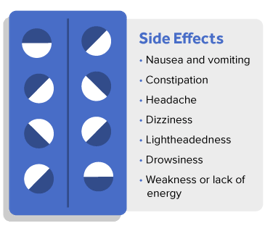
On the other hand, medication noncompliance can be caused by fear of side effects, no proof of improvement, poor tracking of medications, and lack of patient education (i.e., they may not understand why they need to take a prescription).
Finally, beyond definitions and understanding risks and causes, how can providers help patients improve?
Medication Adherence
Medication Compliance
We also can’t ignore that there are different perspectives when it comes to the definitions of medication adherence vs. compliance. For many, the term medication adherence has essentially begun to replace the term and meaning of medication compliance as the latter has fallen out of favor. On the other hand, medication compliance can also represent how well healthcare providers follow rules and regulations for everything from prescribing and administering medications for patients to storing and documenting medications.
Treatment adherence and treatment compliance often appear synonymous. It would stand to reason that if a patient adheres to treatment, that they’re also compliant, right? Not necessarily. Understanding the differences in the meaning behind these two terms is another important aspect of improving medication adherence.
According to the World Health Organization, treatment adherence is defined as, "… the extent to which a person's behavior — taking medication, following a diet, and/or executing lifestyle changes — corresponds with the agreed recommendations from a healthcare provider."
According to the European Society of Hypertension Scientific Newsletter, treatment compliance is defined as, "… the degree to which the patient conforms to medical advice about lifestyle and dietary changes as well as to keeping appointments for follow up and taking treatment as prescribed."
It is important to note that medication adherence/compliance is treatment adherence/compliance specifically focusing on the degree to which a patient conforms to medical advice regarding their medication regimens.
There are several shortcomings associated with treatment adherence and treatment compliance. For example, if patients are faced with the choice of continuing or stopping treatment, they may choose the latter due to financial reasons. Or perhaps as treatment requirements change and patients have to visit new providers, they may not be able to easily travel to new locations and therefore choose not to follow through.
Another challenge is that when patients feel overwhelmed by any number of factors related to treatment, they may choose to not continue. For instance, if patients are unhappy with the treatment’s effects, including limited signs of improvement or unexpected side effects, they may discontinue or not follow through as instructed.
On the other hand, if a patient experiences improvements, they may think that they no longer need to continue treatment.
To help patients with treatment adherence and compliance, here are a few best practices for providers and organizations.
Learn five things to know about medication compliance, including why it is a subject that some healthcare professionals argue is no longer deserving of attention.
Healthcare providers and organizations generally understand that medication adherence is important, but with 50% of patients reportedly not taking their medications as prescribed, there is room for improvement.
Here are a few key reasons hospitals in particular should place a greater emphasis on the importance of medication adherence.
Responsibility to deliver quality care – With nearly 125,000 deaths and 10% of hospitalizations caused by medication nonadherence, hospitals must maintain their commitment to quality care by working to prevent both. Since hospitals play such a significant role in medication adherence, the first steps are to recognize that issues exist and accept that hospitals have a responsibility to help prevent problems in the future.
Reduction in admissions and readmissions – According to one study, 20% of readmission rates occurred in patients with low and intermediate adherence compared with slightly over 9% for patients with high adherence. While the quality of care and patient wellness should be the main reason for improving admission and readmission rates, an additional incentive is the potential for value-based care and financial rewards.

Cost savings – As hospitals spend more while generally being paid less for services, identifying potential cost savings is essential. According to the Annals of Internal Medicine, medication nonadherence costs the healthcare system between $100–$289 billion annually, and there are countless statistics that show similar issues throughout healthcare. If hospitals begin to take steps toward improving medication adherence, there’s great potential to help patients and improve the bottom line simultaneously.


Patient satisfaction – Another important reason hospitals must focus on improving medication adherence is patient satisfaction. As healthcare shifts toward patient-centered models of care, satisfaction is becoming more frequently discussed.
In particular, hospitals shouldn’t ignore the fact that patients have a choice in where they receive medical care. It’s in the hands of hospitals to ensure that patients are achieving and maintaining adherence, which can significantly impact satisfaction. If patients leave the hospital with an understanding of why changes were made to their medication and how to follow the revised regimen while also having their questions addressed, patient satisfaction should improve.

There are several major causes of medication nonadherence, including forgetfulness, questioning of a medication's effectiveness, mistrust of prescriber, fear of side effects, absence of symptoms, and costs. In addition, other causes might be difficulty managing multiple medications, not understanding the purpose of taking a medication, and poor health literacy. Any given cause can be categorized as intentional or unintentional nonadherence, which is an important distinction because sometimes the cause of nonadherence is beyond a patient’s control.
It’s essential that providers understand these causes so they can take appropriate steps to help patients. Here are a few steps doctors can take.
Both types of nonadherence may be caused by lack of patient education. For example, you can offer patients adequate information by giving them a document listing their current prescriptions, providing them with medication instructions, and identifying changes to their treatment. Make sure that you offer any of this information on paper and through an electronic format, and explain how patients should contact you with any questions.
It might go without saying, but you should never assume that patients are taking all of their medications as prescribed. When patients deviate from a regimen, their health is at risk.
To help prevent making assumptions, ask non-judgmental questions. These include the following:
Before speaking with a patient, come prepared with potential solutions to medication nonadherence issues. Consider common issues, suggestions, and support that you can offer to patients. Finally, plan to follow up after appointments to ensure patients are taking advantage of the support you offered.
One group at a higher risk for medication adherence issues is the elderly. Here are a few common challenges and solutions for this group of patients.
Many elderly patients take more than one medication, making adherence even more challenging.
To combat this, doctors can suggest the following to their patients:
Consumer Reports surveys noted that many people skipped filling a prescription, skipped a scheduled dose (without approval), and cut pills in half (without approval) because of cost concerns.
Cost is particularly challenging for elderly patients when they are uninsured, marginally insured, or lack savings. Here are some recommendations to help patients stressing about their financial situations:
Drug interactions with the potential to cause negative or dangerous side effects may discourage patients from continuing taking medications as prescribed. Here are a few ways to address these issues with patients:
Both physical and mental decline in elderly patients can affect medication adherence. For example, if a patient has declining vision, they may not be able to read medication labels as well, affecting their ability to take medications correctly or even at all. Declining ability may prevent patients from picking up prescriptions or refills.
The solution? Address any issues related to vision, strength, and mobility in appointments to help prevent these factors from becoming barriers for patients. Some steps you can take include the following:
Before we dive into the cost of medication nonadherence, there are a few key stats that reveal quite a bit about this issue.
Most of this data comes from a literature review published in the Annals of Internal Medicine in 2012.
In contrast, a newer study from The Annals of Pharmacotherapy states that the annual cost of prescription drug-related morbidity and mortality resulting from non-optimized medication therapy is nearly $530B in 2016 U.S. dollars, with a plausible range of $495 billion to $673 billion.
While the monetary cost is staggering, we can’t neglect to mention the even higher cost of human lives. This study estimates that non-optimized drug therapy results in more than 275,000 deaths annually.
Finally, to round out this chapter, we’ll share some of the top challenges with and solutions for drug adherence.
Many patients do not take medications as prescribed because they lack understanding about the drug itself or how to take it. They might not understand the instructions, or perhaps they take a medication that doesn’t produce an immediate result, which causes them to stop taking it.
The solution? For issues like these and others, healthcare professionals must ensure that they’re educating patients on critical matters concerning medications not just once, but continuously. This may include talking to patients in person during their appointments, providing them with handouts, or sending follow-up emails or texts with the information they need about their medications.
With higher costs in medication becoming all too common, some patients are faced with the difficult choice of paying their bills or paying for medications. This often results in patients choosing not to pick up medications or rationing what they do have, thus not taking the medication as prescribed.
The solution? Physicians must be sensitive to the cost of medications and consider the best, most affordable option when prescribing to patients. You can also offer resources such as NeedyMeds, RX Assistance Programs, state assistance programs, and local agencies that can help. Provide information on these resources via handout or through another communication method, such as links on your website or through email.
Whether real or perceived, the fear of side effects is a legitimate concern that can prevent patients from taking their medications. Perhaps patients begin taking a medication but start to experience an undesirable side effect and decide to discontinue taking it. Or for those with perceived fears, they may believe what they’ve heard from others or read on the internet about side effects, discouraging them from taking their medication
The solution? Ultimately, this goes back to the solution in Challenge #1 above: Physicians must educate patients about potential side effects and alleviate fears by having open and non-judgmental conversations. Along with this, it’s important to check in with patients during each visit to go over medications they’re taking or not taking to hopefully uncover potential issues.
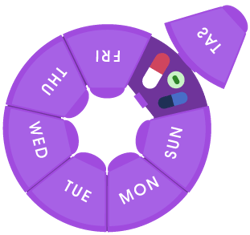
For patients taking multiple medications, following instructions is even more challenging, whether it’s an elderly patient struggling to remember all of their medications or a busy, single parent.
The solution? Consider each patient individually and prescribe medications according to their lifestyle and routine to the best of your ability.
Finally, another major challenge for some patients, whether low income, elderly, or disabled, is transportation.
The solution? Make patients aware of various options they can take advantage of to help secure their prescriptions. For example, Medicaid beneficiaries can access non-emergency medical transport which covers a certain number of rides per month. Or Uber Health, a new service from Uber that provides safe, HIPAA-compliant rides as well as tracking and reporting useful for population health management.
It is imperative that physicians work to help ensure patients fill their prescriptions and take medications as directed. Learn four steps doctors can follow to support these objectives.

The extensive research on medication adherence offers valuable insights into why patients fail to adhere to medications as well as potential solutions for organizations, providers, patients, and caregivers. Here are just a few of the insights from such research.
"Medication Adherence: WHO Cares?" (Mayo Clinic Proceedings) — This 2011 article shares a MEDLINE-based literature search focused on adherence and chronic illness, specifically cardiovascular disease.
1. Patients with chronic illness struggle with adherence.
2. Patients are not solely at fault for medication nonadherence.
3. Patient empowerment can improve adherence.
Medication Adherence: Its Importance in Cardiovascular Outcomes (Circulation) — This 2009 article, which also has a particular focus on cardiovascular disease and outcomes, takes a deep dive into ways of measuring and improving medication adherence.
4. Medication nonadherence by patients isn't always a conscious decision.
5. Patients often improve adherence right before and after an appointment.
Understanding and Overcoming Barriers to Medication Adherence: A Review of Research Priorities (Journal of Managed Care & Specialty Pharmacy) — This 2014 article supplements existing literature on medication adherence with stakeholder interviews and what the researchers describe as "expert" panel meetings. The researchers' goal: "… to improve our understanding about how to identify patients at greatest risk of nonadherence and target them with personalized, effective interventions medication adherence."
6. Factors that drive patient nonadherence aren't always obvious.
7. Technology can help patients improve adherence but is not a cure-all solution.
8. Some improved adherence may not correspond to improved outcomes.
CDC Grand Rounds: Improving Medication Adherence for Chronic Disease Management — Innovations and Opportunities (Morbidity and Mortality Weekly Report (MMWR)) — This 2017 article was published in MMWR, described as the Centers for Disease Control andPrevention's (CDC) "… primary vehicle for scientific publication of timely, reliable, authoritative, accurate, objective, and useful public health information and recommendations."
9. Patients can benefit from multiple adherence strategies.
10. Communication with and education for patients is essential.
Beyond the insights that medication adherence research offers, there are also a number of statistics that shed light on medication adherence challenges and opportunities for providers and organizations.

of people took five or more medicines in 2011-12. Only 8.2% of people took five or more medicines in 1999-2000. (Source)

were due to opioid overdoses in 2016, more than any previous year on record, with an estimated 40% of such deaths involving a prescription opioid.

prescriptions were filled at U.S. pharmacies in 2017. (Source)
Here we identify several research articles on medication adherence and share 10 key lessons learned about patients from these analyses and studies.
Earlier in this guide, we looked at a few definitions of medication adherence. According to a definition from U.S. Pharmacist, "Medication adherence is the act of taking medication as prescribed by a physician. This includes consistently taking the proper dose, at the correct time, and for the recommended length of time."
Looking at this definition, there are a few best practices providers can follow to help patients improve medication adherence.
Finally, beyond best practices, let’s explore a few practical ways to improve medication adherence.
Focus on risks – Emphasizing the risks associated with missing or skipping doses can make all the difference for patients. While the occasional missed dose might not have a negative impact, help your patients understand that their medication is most effective when it’s taken correctly.

Review side effects – When there are unexpected side effects, patients may be more likely to stop taking their medication. In particular, there can be unexpected side effects between over-the-counter drugs and prescriptions, so it’s important to prepare patients in advance.
Give patients a response plan – The conversation about risks and side effects might be stressful for patients, so be sure that you’re ready to discuss a response plan as well. Help them understand what to do if they do miss a dose, how to resolve side effects, and how they can reach someone to ask questions.

Discuss costs – According to a Truven Health Analytics-NPR health poll, cost is the number one reason why patients do not fill prescriptions. Not only may patients stop taking medications due to cost, but they may also ration medications, which means they are not taking them as prescribed. For this reason, be sure to prescribe generic medications when possible and also prepare patients for the approximate cost of a new medication so you can address any concerns about affordability.


Recommend support tools – Finally, offer patients tools that can support medication adherence. This can range from medication calendars to pill organizers to mobile apps. Our next chapter goes into more detail about potential options for tools and apps.
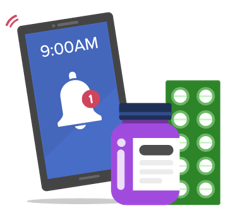
There are number of tools available to help your patients with medication adherence. Here we’ll share just a few highlights of tools worth considering.
There are literally thousands of apps available for patients to help them manage their medications. However, there are very few supported by evidence of effectiveness, which is why we are featuring a few here that go above and beyond.
Now that you have reached the end of this e-book, it's time to put what you've learned to work. You should have a much better understanding of the many contributing factors to medication nonadherence. You also have a wealth of best practices, tools, and tips to leverage as you work to reverse the trend of nonadherence that is likely affecting a majority — or close to it — of your patient population.
Improving adherence in some patients may be as simple as recommending a pill case. Others will require you to address multiple, complex factors, such as affordability, fear, and health literacy. What matters is that you approach each patient and every situation without any preconceived notions. You should also come to appointments with resources in hand that you can leverage to address whatever factors you identify as creating potential barriers to adherence.
As you work with patients, stay optimistic. There is good reason to believe that you can bring about positive changes in your patients' lives, and patients will often respond positively to your enthusiastic outlook. But remain realistic. For as long as medications have been prescribed, adherence has been a challenge. Do not assume interventions will prove successful or remain such. Even when there are fails or setbacks, do not become discouraged. Learn from these experiences so future patients can benefit from your knowledge. It is through such perseverance that we can hopefully eventually say that medication adherence is no longer a significant public health challenge but rather a significant public health success.
© Cureatr 2023 | Privacy Policy
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).