Our guide explores the concept of polypharmacy in great detail, including current trends, risks, challenges and solutions. Read the guide below or enter your email to download your copy to take on the go.
Did you know that more than 40% of older Americans regularly take five or more prescription drugs, and nearly 20% take more than ten medications? The Lown Institute reports:
This is not a new observation. For years physicians and medical experts have been alerting us of the dangers of polypharmacy, which is typically defined as the use of five or more medications.“If nothing is done to change current practices, medication overload will contribute to the premature deaths of 150,000 older Americans over the next decade and reduce the quality of life for millions more.”

To fully understand the topic of polypharmacy, we must first get clear on the definition of the term, which can vary dramatically. We’ve consulted several sources to provide the most comprehensive working definition available, but first, let’s look at the history and evolution of the term.
To break it down to its simplest use, the word “polypharmacy” refers to the use of multiple medications. It follows then that a “polypharmacy patient” is one who has been prescribed and is taking multiple medications for multiple conditions. Let’s review what literature reveals about the nuances of the definition.
A U.S. Pharmacist article illuminates the challenges with defining polypharmacy:
“Although no concrete definition of the term exists, polypharmacy has come to mean the use of several (usually five or more) medications on a daily basis, with the possibility that these may not all be clinically necessary.”
The authors of a BMC Geriatrics article led a systematic review of polypharmacy definitions. They determined that “the most commonly reported definition of polypharmacy was the numerical definition of five or more medications daily.”
The World Health Organization (WHO) backs up this definition and furthers it with more detail. WHO has defined what qualifies as a "medication” in its definition, stating,
“Polypharmacy is often defined as the routine use of five or more medications. This includes over-the-counter, prescription and/or traditional and complementary medicines used by a patient.”
In addition to the term being most used to describe the number of prescriptions being taken, polypharmacy is sometimes used to indicate that a patient may be on too many or unnecessary medications. In fact, many physicians have begun adopting a philosophy of “deprescribing.” In these cases, step-down methods, tools, and new approaches are used with patients to remove or reduce doses of medicines that are inappropriate, duplicative, or unnecessary. Involving a clinical pharmacist in the conversation is often part of the process of deprescribing.
As with any medication regimen, there are both benefits and risks associated with polypharmacy. To be sure, when it’s medically necessary, patients taking multiple medications — even five or more daily — can benefit greatly from the proper mix. In fact, adhering to the best mix of medications can help manage chronic conditions, treat ailments, and improve a patient's quality of life. In other words, no small benefit.
However, there’s a big caveat. The key to achieving such benefits is through “intelligent polypharmacy,” which relies on access to accurate data about prescriptions. Alternative terms for intelligent polypharmacy also include “rational polypharmacy,” “targeted polypharmacy,” "evidence-based polypharmacy,” and “combination pharmacotherapy.”
While it may seem straightforward, there are many factors that can stand in the way of attaining the benefits associated with polypharmacy. Ideally, effective polypharmacy should boil down to the same guidelines that should exist for any medication regimen: patient- and condition-specific medication selection together with effective review of interaction risks and ongoing medication management, reconciliation, and deprescribing (where appropriate). All these steps help ensure optimization of the regimen.
Although the number of medications a patient is taking is an important consideration for effective medication management, it’s not the most important factor. To truly optimize the regimen, you’ll need an understanding of the value of each medication individually and the role it plays within the regimen in helping realize health and wellness goals. Sound prescribing decisions will make this consideration a higher priority.
There are several risks associated with polypharmacy. Here, we examine three of the main ones:

Increasing the number of medications – Increasing the number of medications, logically, increases the potential for adverse drug events (ADEs) and adverse drug interactions. In fact, this is one of the biggest risks of polypharmacy. As an Expert Opinion on Drug Safety article notes, a population-based study showed that outpatients taking five or more medications had an 88% increased risk of experiencing an ADE compared to those who were taking fewer medications.

Increasing the number of medication adherence challenges – Increasing the number of medications also expands medication adherence challenges. Naturally, increasing the number of medications creates more management challenges for patients, thus increasing the likelihood of medication nonadherence.

Increased healthcare costs for patients and the healthcare system – Polypharmacy has also been shown to contribute to increased healthcare costs for patients and the healthcare system. As Bloomberg reports, Americans spend more on prescription drugs than anyone else in the world, with average costs of about $1,200 per person per year. As a patient's number of medications rises, so typically do their out-of-pocket costs. If the patient is covered by federal or government-subsidized insurance, some of those costs are likely incurred by taxpayers. Adding to the risks is that millions of patients are reportedly skipping medications due to their high cost, which can ultimately create even worse health and safety outcomes for patients and the healthcare system.

Considering that polypharmacy is on the rise and carries with it significant risks, it’s clear that healthcare organizations must develop guidelines for their approaches to polypharmacy management in order to be responsible. This includes identifying a baseline of polypharmacy guidelines and strategies to inform decisions concerning policies and procedures.
Here we examine samplings of what recent literature has to say regarding polypharmacy guidelines and strategies, specifically for certain patient population groups and practitioners as well.
From Clinical Cardiology:
“The impact of polypharmacy in older adults can range from reduced quality of life to serious adverse drug events. Most would agree that striking a balance between over‐ and under‐treatment is important, yet doing it effectively is challenging due to the lack of clear guidance and insufficient clinical experience.”
From UpToDate:
“It is particularly important to reconsider medication appropriateness late in life. A model for appropriate prescribing for patients late in life has been proposed. The process considers the patients' remaining life expectancy and the goals of care in reviewing the need for existing medications and in making new prescribing decisions.”
From U.S. Pharmacist:
“… healthcare providers must evaluate each drug and balance its potential adverse effects against its potential benefits. Advances in information technologies such as electronic prescribing, electronic medical records, and electronic laboratory results, will help prevent adverse drug effects and interactions.”
From BMJ Open:
“… patients with diabetes and polypharmacy may benefit from multidisciplinary collaborative care model that involves pharmacist follow-up for the patients to assess the medication use and minimize polypharmacy.”
From American Nurse:
“Although glycemic targets for type 2 diabetes are well established, intensive management can lead to adverse outcomes in older adults. For adults with limited life expectancy or severe comorbid illness such as frailty or dementia, aiming for a glycated hemoglobin of < 8.5% is reasonable. For older adults at high risk for hypoglycemia, or for whom hypoglycemia would be detrimental, choosing agents unlikely to promote hypoglycemia is warranted. In some situations, de-intensifying or deprescribing therapy in older adults is necessary. In addition to de-intensifying regimens, choosing those that are less likely to cause adverse reactions is important.”
From Journal of the American College of Cardiology:
“From the Journal of the American College of Cardiology: Building efficient communication lines between and within teams is the key to successful co-management of cardiovascular and noncardiovascular medications. For example, if the cardiologist identifies a high-risk or overtly harmful noncardiovascular medication, then the cardiologist can:
From Medscape:
“To prevent and resolve nonadherence and polypharmacy in patients with heart failure, clinicians should utilize available resources from their own societies as well as patient-education-based programs to develop a shared decision-making, multidisciplinary approach — one that includes dedicated time to identify specific values and preferences of the patient, as well as barriers to medication adherence.”
The recommendations from literature also include general guidelines for pharmacists and prescribing entities. These best practices should be considered as a component of your organization's polypharmacy management plan.
From U.S. Pharmacist:
“Pharmacists need to identify drug-related problems, prioritize them, reduce pill burden, eliminate unnecessary medication usage, and monitor for adverse drug-withdrawal events. Pharmacists can optimize medication therapy and improve therapeutic outcomes for patients through medication therapy management (MTM).”
From Aging Medicine:
“The clinical pharmacist has a major role to play in selecting the best interventions needed to enhance suitable polypharmacy and consequently managing problems associated with polypharmacy properly to accomplish better clinical results for patients.”
From American Journal of Health-System Pharmacy:
“Pharmacists play a significant role in preventing ADEs by critically analyzing the medication list and discontinuing (or recommending discontinuation of) medications that do not provide effective disease control or whose use results in ADEs.”
From Psychiatric Times:
“There is a need for proper clinical titration, sound treatment algorithms, and well-defined protocols to effectively reduce irrational polypharmacy. An important clinical issue is when a patient on multiple drugs presents to a psychiatrist who wants to change the prescriptions to another multiple-drug combination. It is important that certain drugs from the previous prescriptions be retained so that a switch can be made. Tapering medication must be done at a gradual rate while closely monitoring for withdrawal/rebounding symptoms. When changing a medication, it is wise to switch the medication with one that has a similar half-life to enhance continuity of action.”
Clearly, pharmacists have an opportunity to greatly affect medication therapy management for polypharmacy patients. Enabling easy accessibility and transparency into a patient’s drug regimen can empower pharmacists to take a greater role in mitigating some of the risks inherent in polypharmacy.
Optimal polypharmacy management is achieved with these 8 deprescribing guidelines.

Now that you have an understanding of the definition of polypharmacy and what the research has said about guidelines for mitigating risks, let’s take a closer look at the recent trends and developments related to the topic.
When it comes to understanding the depth and breadth of polypharmacy’s impact on older adults, one needs to look no further than the statistics. The numbers we’ve cited from recent sources create a narrative that words alone don’t quite capture. Let’s examine a few:
67% of older people – A study published in JAMA Internal Medicine found that the number of older people taking five or more prescription drugs, over-the-counter medications, and supplements is about 67% — a figure that, like many alarming polypharmacy metrics, is on the rise.
150,000 premature American deaths and more than 4.6 million hospitalizations – The Lown Institute, in an April 2019 report, estimated that polypharmacy — which Lown essentially refers to as “medication overload” — would result in 150,000 premature American deaths and more than 4.6 million hospitalizations over the next decade. “[Medication overload] will reduce the quality of life for millions more. Strong, coordinated, and immediate action is needed to stem the tide of this epidemic, which harms people of all ages, but especially older generations.”
A 58% risk of ADEs – In a study, polypharmacy was shown to increase the risk of adverse drug events, or ADEs, from 13%, which is associated with taking two medications, to 58%, which is associated with five drugs. When patients are taking seven or more medications, the risk of ADEs surpasses 80%.In fact, The Lown Institute notes that the risk of an ADE increases by 7–10% with each medication.
Most experts agree that while polypharmacy is associated with health and wellness risks, it’s not a good idea for clinicians to just arbitrarily reduce polypharmacy in older adult patients. Empowering practitioners and patients with resources and tools (combined with a focus on deprescribing) makes it possible to dramatically reduce the risks of polypharmacy while also keeping patients safe.
Examine six ways telepharmacy is adding value for patients in our healthcare delivery system.
In general, the discussion about polypharmacy revolves around “older adults,” defined as those at least 65 years of age. Let’s review some of the most commonly discussed challenges, including adverse effects, medication adherence issues, and — most recently — the impacts of the COVID-19 pandemic.
Because the aging process naturally makes one more vulnerable to adverse effects, any discussion of polypharmacy challenges inherently leads back to the elderly, even though people of any age can be polypharmacy patients. When kidney and liver function decline as a normal part of the aging process, it’s harder for the body to flush itself of medications and other toxins in the body as we get older. As a result, medications accumulate faster in the system of an older patient than they would in a healthy, younger person.
When this normal aspect of growing older is amplified with seven, nine, or more medications, this puts the patient at risk for negative outcomes, such as adverse events or side effects.
In addition, polypharmacy has been associated with non-adherence in older adults because, quite simply, it’s complicated for them to manage. This can inevitably lead to some dangerous outcomes: Patients are more likely to experience adverse drug events (e.g., drug reactions, allergic reactions, overdoses, and missed doses) when they struggle with medication management — especially when the number of medications increases.
Also, older patients are more likely to experience adverse drug events. It gets even more complicated when a medication regimen undergoes changes — this scenario puts patients in particular danger of experiencing adverse drug events. When a regimen becomes more complex with the introduction of additional and new medications, it becomes more difficult to develop and maintain a medication routine.
And changes to a regimen are not often well informed. Often patients receive prescriptions from multiple prescribers who do not have access to or effectively review a patient's medication regimen prior to making changes to it, and this raises the risk for some of the previously mentioned adverse drug events. Many times, prescribers and pharmacies don’t communicate about those patients they have in common. Even when the prescribers and pharmacists have the best intentions, they can be deterred by a lack of time, resources, and information to reliably piece together an accurate medication list for patients.
Another contributing factor that increases the risk of adverse effects is the failure to perform medication reconciliation post-discharge (MRP), which can result in medications remaining a part of a regimen for longer than necessary. Failure to adequately and consistently perform medication reconciliation is one of the quickest paths to patient and caregiver confusion about the proper medications a patient should take. Such confusion can lead to medication errors and harm. In contrast, proper medication reconciliation helps to decrease or eliminate medication discrepancies.
Lastly, with more patients using dietary supplements, the risks associated with them is generating increased attention — an article in the Evidence-Based Complementary and Alternative Medicine journal states, cases of excessive or inappropriate use of herbal dietary supplements have even led some to coin the term “polyherbacy,” a designation associated with some of the health problems associated with polypharmacy.
Along with adverse effects and their corresponding danger, polypharmacy also comes with the aforementioned medication adherence challenges. Let’s examine why that is in more detail.

Complex dosing schedule – More prescriptions mean a more complex dosing schedule as well. Even if patients utilize a calendar to schedule doses, they may still experience occasional poor compliance or confusion with dosing.


Medication instruction confusion – Since all medications come with lengthy directions that spell out the amount of medicine to take, how to take it, dosing schedule, and when not to take the drug, polypharmacy patients have the potential for getting confused. They are likely to mix up the rules for these medications, particularly when multiple medications appear the same (e.g., inhalers, injections, similarly colored pills) or have a similar sounding or looking name (i.e., look-alike and sound-alike drugs).

Side effects – Even side effects associated with some medications can create issues with adherence compliance. If a patient is taking a medication that causes fatigue and lethargy, he or she could sleep through a dosing period. Also, some medications cause memory loss, causing a patient to forget when to take medications or believing they have not yet taken a medication, which can lead to double (or more) dosing.


Reactions – The more medications that prescribers must factor in, the more likely it is that they will have trouble predicting reactions. Though prescribers have tools that can help predict possible adverse drug reactions between medications, they often don’t make up for the fact that polypharmacy raises the risk that medications taken together will lead to undesirable (and potentially harmful) interactions.


High cost – Sometimes the reason for nonadherence comes down to finances. Naturally, more medication usually translates to greater costs for patients, which can add up quickly when you factor in refills. Inevitably, patients who have financial limitations may not fill or refill a prescription or postpone doing so.


Fill and refill frequency – Some patients may have difficulty travelling to visit a pharmacy to fill or refill their prescriptions. Challenges are further magnified when patients are expected to fill and then refill numerous medications, especially when the timing of filling and refilling medications are not consolidated and require multiple trips to a pharmacy.

In the scope of polypharmacy challenges, the stress of the recent pandemic cannot be underestimated. In summary, the pandemic has taken a significant mental health toll on people, which has translated to substantial increases in medication use. For instance, consumer use of antidepressant, anti-anxiety, and anti-insomnia medications are on the rise, reported Express Scripts. And extended time indoors and being less active led many to treat ailments such as headaches and backaches. Additionally, during this time, consumers have also increased their usage of dietary supplements by taking the same supplements more regularly and increasing doses.
With increased medication use, patients often fill medications at more than one pharmacy, upping the potential for several risks, including medication duplication, drug-drug interactions, and complex medication management. A U.S. Pharmacist article addresses the challenges created by this, stating,
“Pharmacists provide more efficient medication therapy management (MTM) services when they have a complete picture of the patient's health status.”
When multiple pharmacists at multiple pharmacies do not have access to information from one another, it can negatively impact patients’ health.
Complicating matters even more is that the COVID-19 pandemic prompted many people to begin using mail-order pharmacies to reduce the need to leave their homes and travel to physical pharmacies to pick up prescriptions. While mail-order prescriptions have helped patients limit their exposure to the novel coronavirus, it has also introduced another “pharmacy” into the equation for many patients. And medications delivered by mail bring their own risks.
Lastly, during this time, some people have changed doctors, which can easily lead to miscommunication between the parties. New physicians are, naturally, unfamiliar with patients, and many times they may not have easy access to a patient's medical and medication history.
And in some cases, the pandemic has prompted doctors to change their plans or employers. A physician survey conducted by Jackson Physician Search explains that “54% of physicians surveyed said COVID-19 has changed their employment plans. Of those, 50% are considering leaving for a new healthcare employer, 21% said they may hang up their white coat for early retirement, and 15% are thinking about leaving the practice of medicine entirely.”
With the risks and inherent dangers that come with polypharmacy, it makes sense to examine ways to mitigate the harmful effects while developing guidelines that chart a healthier course for patients.
Here are five causes of polypharmacy in the elderly as well as some commentary about the dangers associated with each cause.
Fortunately, the healthcare industry has made concerted efforts to develop tools that can help tackle the challenges inherent to polypharmacy. One important way they are tackling the challenges is through deprescribing, defined as using step-down methods and tools to remove or reduce doses of medicines that are inappropriate, duplicative, or unnecessary.
By using one or more of the following tools, your organization can help safely reduce polypharmacy, increase deprescribing, and help patients achieve substantial clinical and financial benefits.
“The MAI is designed to allow rating of 10 explicit criteria to determine whether a given medication is appropriate for an individual. The ten criteria of the MAI, worded as questions, pertain to the individual patient and drug in question.”
Each criterion is rated on a three-point Likert scale. When added up, the resulting score is intended to determine the level of inappropriateness, with a score of 0, meaning the drug is appropriate, and 18 representing maximal inappropriateness.
“… compendium of medications potentially to avoid or consider with caution because they often present an unfavorable balance of benefits and harms for older people.”
With the STOPP/START criteria, clinicians can potentially decrease polypharmacy by improving medication appropriateness.“Unlike the Beers Criteria, STOPP and START criteria provide guidance on inappropriate medications as well as medications that are underprescribed.”
Tools are not the only effective means of preventing or better managing polypharmacy — physicians themselves can adopt better practices as well. Let’s review some ways they play a role.
Even though medications are typically recommended by well-intentioned providers or clinicians, the sheer number of them increases the potential for drug-drug interactions, side effects, and other adverse events. It’s the volume and frequency that make it imperative for physicians to consider ways to prevent or at least improve the management of patient polypharmacy.

Be diligent about medication reconciliation – A physician should first create a complete and accurate list of all medications a patient is taking. In reality, this may not be an easy task. For example, in an emergency department or at inpatient admission, collecting a complete list that includes reason, dosage, and frequency can take hours that doctors may not have. However, conducting an accurate reconciliation is vital to patient safety and care. The danger is that patients admitted with an incomplete or inaccurate medication list may be prescribed duplicate medications or medications that can interact with an existing regimen. As a result, patients may experience an interaction or adverse drug event during or after a hospital stay.

Ask patients the right questions – Specifically, doctors should inquire if they are being treated by other physicians. In reality, patients taking multiple medicines to manage multiple conditions are most likely being treated by multiple specialists and other providers. Unknowingly, each provider may take a condition or disease-centric approach to prescribing. Also, patients may not understand that the cardiologist needs to know about the pills that the pulmonologist and orthopedist prescribed or vice versa.

Verify there is a use for every medication– Though this seems obvious, every medication must map to a diagnosis or other indication and be clearly communicated to the patient, along with the reason for taking it. If this cannot be established, physicians should inquire about why the patient is taking the medication in the first place.

Evaluate deprescribing opportunities – By conducting a systematic, one-on-one review of polypharmacy patient regimens, physicians can set the goal of simplifying, deprescribing, or modifying medication regimens while still maintaining efficacy. This will require doctors to ask questions about the purpose of each medication.

Include a pharmacist in the discussion – Pharmacists need to be involved because they can provide insights into a patient’s regimen from a pharmacologic perspective. Also, they will be able to recommend medications that can be removed and/or dosages that should be modified.

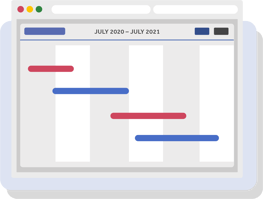
Use technological tools to deliver accurate prescription data – Cureatr’s Meds 360° is an example of a tool that provides physicians with accurate real-time medication data derived from data feeds of actual pharmacy purchases. In one 12-month view, providers can see which prescriptions, by therapeutic class, a patient has filled or not filled, dosage changes, duplicate medications, and more. Data like this helps to bridge patient memory gaps and EHR inconsistencies, making it easier for physicians to determine which medications the patient may or may not need to continue taking.

Use behavior modification – Examples of patient behavior modification include exercise and dietary changes for patients with diabetes or certain cardiovascular conditions, art and music for patients with dementia or depression, or cooking classes for patients with diabetes or obesity. Additionally, many residential communities offer programs that include pets and aromatherapy or learning opportunities for residents. By encouraging activities like these, physicians can help provide an opportunity for condition improvement without drug intervention.
To help with deprescribing, practitioners turn to frequently cited guidelines. Five often referenced guidelines were developed by the Bruyère Research Institute Deprescribing Guidelines Research Team and collaborators. These guidelines, along with other resources, are available on the Bruyère's website, deprescribing.org. Many of the guidelines described below pertain to certain medications, giving instructions specifically tailored to safely tapering or discontinuing the said medication.
“First, work with your healthcare provider to choose appropriate blood sugar and A1C targets for your age and state of health … Together, develop a plan for medication changes. This might involve reducing a dose, changing to a safer medication, or stopping a medication altogether. Such changes could occur every 1-2 weeks, always under the supervision of your healthcare provider.”
“For BPSD symptoms, slowly reducing the dose of an antipsychotic over several weeks is recommended. This allows healthcare providers to carefully monitor for any return of symptoms. If used in low doses for insomnia, antipsychotics can be stopped completely without first reducing the dose.”
Patients are advised to check for and report signs of psychosis, aggression, agitation, delusions, and hallucinations When reducing an antipsychotic used for BPSD. Note that the reduction of an antipsychotic used for insomnia is not typically associated with withdrawal symptoms.
“It stresses that deprescribing should begin as a trial discontinuation, with close periodic monitoring (e.g., every four weeks). The dose of ChEI/memantine should be tapered by halving the dose or by stepping down through available dose formulations every four weeks to the lowest available dose, followed by discontinuation.”
“Reducing the dose might involve taking the PPI once daily instead of twice daily, lowering the number of mg (e.g., from 30mg to 15mg, or 40mg to 20mg, or 20mg to 10mg depending on the drug), or taking the PPI every second day for some time before stopping.”
One of the best ways to address the risks of polypharmacy is the move toward deprescribing, as previously mentioned. As deprescribing.org explains, the term refers to more than just reducing doses of unnecessary medications or discontinuing them— it has to be planned and supervised carefully.
In fact, as more people understand the benefits of this push, it’s fair to say that deprescribing has become a worldwide movement. The European Journal of Hospital Pharmacy explains why:
“Unprecedented levels of polypharmacy, especially in the (older) population, combined with increases in patient harm and adverse drug events due to condition-drug and drug-drug interactions leading to morbidity and mortality are key drivers for a deprescribing movement.”
In the U.S., the KHN report cites that support for the movement has been reinforced by physician-led efforts, such as the Choosing Wisely campaign.
It’s widely recognized that by safely decreasing patients’ medication burden, you can deliver crucial benefits, not the least of which is helping patients better manage their medication regimen, improving medication adherence. This is due to the fact that deprescribing simplifies patient's medication management process because they have more time to adapt and allocate time to better management and adherence.
However, deprescribing doesn’t just simplify medication management. It can positively impact a patient's finances by reducing the number of medications they need to purchase, the time they need to spend filling and refilling medications, and the likelihood they will need expensive urgent or emergent care due to safety risks. And the savings can then be passed along to the healthcare industry. Just consider that suboptimal medication management drives $528 billion of unnecessary costs and contributes to 275,000 deaths annually. A great deal of these costs and outcomes are attributable to unnecessary therapy.
Despite its clear benefits, deprescribing is not without challenges. Some of the persistent obstacles that can be overcome include the following:
As with most challenges, the path to overcoming these obstacles begins with education. When patients and prescribers are informed about the benefits of deprescribing, they are more likely to be receptive to the idea.
The key to making patient and prescriber education successful is empowering them with the right tools to enact real change. One such tool is Cureatr’s Meds 360°. Using this tool, physicians can access accurate real-time medication data derived from data feeds of actual pharmacy purchases. This kind of visibility allows insight that can lead to educated prescribing choices. For example, in one 12-month view, providers can see which prescriptions, by therapeutic class, a patient has filled or not filled, dosage changes, duplicate medications, and more.
Having this kind of data doesn’t just help physicians. This kind of comprehensive information can help to fill patient memory gaps and EHR inconsistencies. As a result, it becomes easier for physicians to determine which medications the patient may or may not need to continue taking.
As physicians have begun adopting a philosophy of “deprescribing,” many are realizing the value of including a clinical pharmacist in the conversation.
Cureatr’s Meds360 platform employs dedicated board-certified pharmacists who can assess patients, evaluate medication therapies, develop medication care plans, and handle follow-up and monitoring. In essence, this tool enables them to become an extension of your care team.
It is imperative that physicians work to help ensure patients fill their prescriptions and take medications as directed. Learn four steps doctors can follow to support these objectives.
Until now, clinicians have had significant barriers to access a patient's current, comprehensive medication list that includes drug information from all prescribers and retailers. But that has changed as the future of polypharmacy has begun to focus on intelligent polypharmacy. By offering clinicians a complete medication picture, we can begin to break through the hesitation to perform the deprescribing process driven by fear of making a change to a regimen that could have unintended consequences.
The potential benefits of this solution are numerous and weighty. Not only does can it save countless dollars for the healthcare industry, it can save the lives of many Americans.
With Meds 360° from Cureatr, an industry-leading medication management platform, users can now view the past 12 months of a patients' medication history. Such features give patients, as well as physicians and prescribers, incentive to be more engaged in comprehensive medication management. The platform also includes alerts to dangerous drug combinations, therapeutic duplications, and dose changes that can identify threats associated with polypharmacy, help assess medication adherence, and support data-based care decisions, including those concerning deprescribing.
To learn more about how Meds 360° is helping clinicians nationwide more easily and efficiently perform deprescribing and do so with confidence, schedule a demo.
© Cureatr 2023 | Privacy Policy
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).